The Link Between Stress, Gut Health and Anxiety
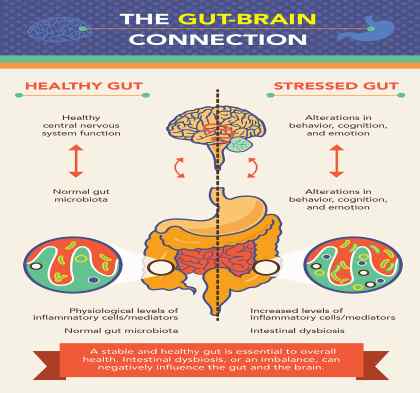
Understanding the Gut–Brain Connection
Your gut and brain are in constant conversation. When anxiety rises, many people feel it immediately in the body. A tight or heavy stomach. Nausea. Fluttering sensations. Reflux that appears during stressful weeks. IBS flare ups that seem to arrive without warning.
What is less widely understood is that this relationship also works in reverse. Ongoing digestive imbalance can actively drive anxiety, low mood, fatigue, irritability, panic sensations, brain fog, and emotional overwhelm.
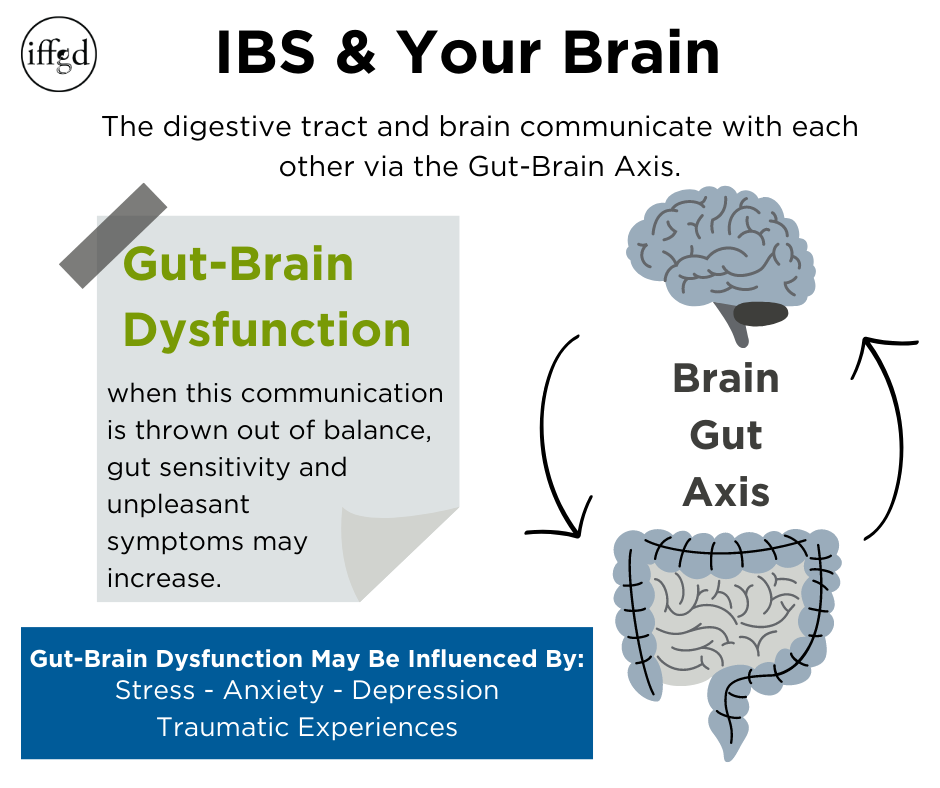
This two way communication is known as the gut–brain axis. It explains why chronic stress so often shows up as digestive symptoms, and why unresolved gut issues can keep anxiety patterns stuck in place.
At Counselling Experts, support is provided through Counselling and Psychotherapy, RTT®, Clinical Hypnotherapy, Clinical Medical Hypnotherapy, and Registered Nutritionist Services. This integrated, evidence informed approach works with both the nervous system and digestive system, helping restore calm, clarity, emotional regulation, and steadier energy.
Appointments are available ONLINE nationwide and in person across Limerick, Adare, Abbeyfeale, Newcastle West, Midleton, Youghal, Charleville, Kanturk, Cork, and Dublin.
Understanding the Gut–Brain Axis
The gut–brain axis is not a metaphor. It is a well researched biological system linking the digestive tract and the brain through nerves, hormones, immune signals, and gut bacteria.
The gut contains its own nervous system, called the enteric nervous system, made up of more than 100 million nerve cells. It also produces over 90 percent of the body’s serotonin, a neurotransmitter involved in mood stability, sleep, appetite regulation, pain perception, and emotional balance.
Because of this close connection, anxiety does not live only in thoughts. It is experienced throughout the body. When stress disrupts digestion or gut bacteria, signals travel back to the brain via the vagus nerve, amplifying anxious sensations, panic symptoms, low mood, irritability, and cognitive fog.
How Stress Disrupts Digestive Function
When the brain perceives threat, the body activates the fight or flight response. Blood flow is diverted away from digestion and toward muscles and survival systems. This response is protective in short bursts, but damaging when stress becomes chronic.
Ongoing stress alters stomach acid production, slows digestive enzymes, changes gut motility, and interferes with nutrient absorption. Over time, this creates digestive instability.
Common stress related gut symptoms include:
• IBS symptoms
• Bloating and abdominal distension
• Acid reflux and heartburn
• Constipation or diarrhoea
• Cramping and abdominal pain
• Nausea after eating
• Loss of appetite or overeating
• Food sensitivities during stressful periods
Large clinical studies show that people with IBS have significantly higher stress hormone levels, particularly cortisol, and that reducing psychological stress through therapy leads to meaningful symptom improvement.
How Gut Imbalance Can Worsen Anxiety
The gut microbiome, your internal ecosystem of bacteria, plays a direct role in emotional regulation. Certain gut bacteria produce calming compounds such as GABA and short chain fatty acids, which support mood, focus, and stress resilience.
Chronic stress, illness, restrictive eating, antibiotics, and inflammation can reduce these beneficial bacteria. When this balance is disrupted, the gut sends distress signals to the brain.
People may experience increased anxiety, low mood, emotional volatility, panic sensations, fatigue, brain fog, poor sleep, and reduced stress tolerance, even when life circumstances seem manageable.
Counselling addresses the emotional drivers of gut stress. Nutrition support rebuilds gut balance from the inside. Together, they help break the reinforcing cycle between anxiety and digestion.
The Emotional Side of Digestive Symptoms
Many clients describe “holding stress in their stomach”. This is not imagined. Emotional tension often shows up physically as a tight chest, clenched jaw, shallow breathing, or an unsettled gut.
These physical reactions are part of the body’s emotional signalling system. When feelings such as fear, anger, sadness, or overwhelm are unrecognised or suppressed, the body often expresses them instead.
Counselling and Psychotherapy help you recognise emotional triggers earlier, understand patterns such as perfectionism, people pleasing, chronic responsibility, or burnout, and express emotions safely rather than carrying them internally.
As emotional awareness improves, digestive symptoms often ease.
Counselling for Anxiety, Stress, and Gut Symptoms
Counselling focuses on present day stressors and how they affect both emotional wellbeing and physical health.
Many clients with IBS, reflux, bloating, or nausea are also living with ongoing work stress, relationship strain, caregiving pressure, or chronic emotional overload.
Counselling supports the gut–brain axis by reducing nervous system activation, improving emotional awareness, identifying stress patterns, and supporting healthier boundaries.
As the nervous system settles, digestion often becomes steadier and anxiety softens.
Psychotherapy for Long Standing Gut–Brain Patterns
Psychotherapy works at a deeper level, exploring why stress responses became embedded in the nervous system.
Clients with long term digestive symptoms often describe a lifetime of tension. Many were told their symptoms were “just stress” without support to understand where that stress originated.
Psychotherapy addresses deeper emotional themes such as early responsibility, unresolved grief, betrayal, or prolonged emotional suppression. These experiences can keep the nervous system in a state of vigilance, directly affecting gut function, inflammation, and hormone regulation.
RTT®, Advanced Rapid Transformational Therapy, and Subconscious Stress Responses
RTT® (Rapid Transformational Therapy) and advanced RTT works with the subconscious mind, where automatic stress responses are stored.
The subconscious controls gut tension, urgency, panic sensations, and digestive shutdown. Even when stress is understood intellectually, the body may continue reacting as if danger is present.
RTT® helps identify and reframe the root experiences that taught the nervous system to stay on high alert, supporting calmer gut–brain signalling.
Clinical Hypnotherapy and Clinical Medical Hypnotherapy
Clinical Hypnotherapy and Clinical Medical Hypnotherapy have strong evidence for IBS, Gut issues, Digestive issues, anxiety, and stress related digestive conditions.
Under chronic stress, the gut becomes hypersensitive. Normal sensations are interpreted as threat, leading to pain, urgency, reflux, or nausea. Hypnotherapy helps recalibrate gut sensitivity and calm the autonomic nervous system.
Clinical Medical Hypnotherapy is particularly helpful when digestive symptoms are closely linked to anxiety, panic attacks, trauma responses, or medical stress.
Registered Nutritionist Services and Gut–Brain Chemistry
Nutrition plays a central role in gut–brain communication. The gut microbiome influences neurotransmitters, inflammation, blood sugar regulation, and hormone balance.
Stress often disrupts appetite, digestion, and food tolerance. Many clients restrict foods during flare ups, unintentionally increasing stress on the system.
Registered Nutritionist support focuses on restoring balance rather than restriction. This includes supporting gut bacteria, stabilising blood sugar, reducing inflammation, and improving nutrient absorption.
When nutrition is aligned with emotional regulation work, progress is often faster and more sustainable.
Why an Integrated Approach Matters
Anxiety and gut symptoms rarely improve when only one layer is addressed. Talk based therapy alone may not settle gut sensitivity. Nutrition alone may not calm a nervous system shaped by years of stress.
When Counselling, Psychotherapy, RTT®, Clinical Hypnotherapy, Clinical Medical Hypnotherapy, and Registered Nutritionist Services are personalised to your needs, and combined thoughtfully, the gut and brain receive consistent signals of safety rather than threat.
Clients report fewer flare ups, improved digestion, reduced anxiety, better sleep, steadier energy, and clearer thinking.
Book Your Private Consultation
If anxiety, IBS, bloating, reflux, fatigue, panic sensations, or emotional overwhelm are affecting your quality of life, support is available.
Appointments are offered ONLINE nationwide and in person across Limerick, Adare, Abbeyfeale, Newcastle West, Midleton, Youghal, Charleville, Kanturk, Cork, and Dublin.
Book your consultation today and begin restoring calm, balance, and confidence.
Frequently Asked Questions
1. Can stress really cause gut problems?
Yes. Stress hormones slow digestion, alter gut bacteria, and increase gut sensitivity.
2. Why does anxiety show up in my stomach?
The gut and brain communicate through the vagus nerve. Anxiety triggers gut muscle tension.
3. Can gut problems worsen anxiety?
Yes. An inflamed or imbalanced gut sends distress signals to the brain.
4. What is the gut–brain axis?
It is the two way communication between the digestive system and the brain.
5. Can counselling help IBS?
Yes. Counselling reduces stress driven nervous system activation.
6. How is psychotherapy different from counselling?
Psychotherapy explores deeper emotional patterns behind chronic symptoms.
7. Does hypnotherapy help digestive issues?
Yes. Clinical Hypnotherapy is evidence based for IBS and gut sensitivity.
8. What is Clinical Medical Hypnotherapy?
It integrates hypnotherapy with medical understanding of stress related conditions.
9. Can RTT® help anxiety and gut symptoms?
Yes. RTT® addresses subconscious stress responses affecting digestion.
10. Can nutrition improve anxiety?
Yes. Gut bacteria influence neurotransmitters involved in mood.
11. Why do gut symptoms flare under stress?
Stress diverts resources away from digestion.
12. Can therapy help reflux?
Yes. Stress reduction often eases reflux symptoms.
13. Is IBS linked to anxiety disorders?
Yes. IBS commonly coexists with anxiety.
14. Can trauma affect digestion?
Yes. Trauma can keep the nervous system hyper alert.
15. Why do I feel bloated when anxious?
Stress alters gut motility and sensitivity.
16. Does poor sleep affect gut health?
Yes. Sleep disruption worsens gut and mood regulation.
17. Can online therapy help gut anxiety?
Yes. Online therapy is effective nationwide.
18. How long does improvement take?
Many notice changes within weeks, with deeper progress over months.
19. Are probiotics helpful?
Some strains may help, best chosen with guidance.
20. Can therapy reduce panic attacks linked to gut symptoms?
Yes. Therapy teaches grounding and regulation skills.
21. Is gut health linked to fatigue?
Yes. Inflammation and poor absorption affect energy.
22. Can stress cause food intolerances?
Stress can increase gut sensitivity to foods.
23. What role does inflammation play?
Inflammation disrupts gut barrier and neurotransmitters.
24. Can counselling improve emotional eating?
Yes. Emotional regulation reduces stress eating patterns.
25. When should I seek professional support?
If gut symptoms persist alongside anxiety, sleep problems, or low mood.
Key Scientific References
Mayer EA. Gut–brain communication. Nature Reviews Neuroscience. 2011. https://doi.org/10.1038/nrn3071
Cryan JF, Dinan TG. Mind altering microorganisms. Nature Reviews Neuroscience. 2012. https://doi.org/10.1038/nrn3346
Ford AC et al. Irritable bowel syndrome. The Lancet. 2017. https://doi.org/10.1016/S0140-6736(16)31548-5
Slavich GM, Irwin MR. Stress and inflammation. Psychological Bulletin. 2014. https://doi.org/10.1037/a0035302
Chrousos GP. Stress system disorders. Nature Reviews Endocrinology. 2009. https://doi.org/10.1038/nrendo.2009.106
Segerstrom SC, Miller GE. Psychological stress and immunity. Psychological Bulletin. 2004. https://doi.org/10.1037/0033-2909.130.4.601
Tracey KJ. The inflammatory reflex. Nature. 2002. https://doi.org/10.1038/416003a
Carabotti M et al. Gut–brain axis. Annals of Gastroenterology. 2015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/
Clarke G et al. Gut microbiota and stress. Molecular Psychiatry. 2013. https://doi.org/10.1038/mp.2012.135
Educational Disclaimer
This article is for educational purposes only and does not replace medical advice. Always consult your GP or healthcare provider before changing treatment or medication.